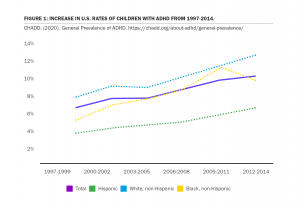
It is a challenging time for an increasing number of U.S. patients with behavioral health disorders. More than 10% of youth in the U.S. are diagnosed with ADHD,11 and 64% of these children have at least one additional behavioral, emotional, or mental health disorder.22 Furthermore, ADHD is on the rise in the United States. The overall rate of ADHD in children aged 2-17 has increased from 6.1% to 10.2% since 1998 (see Figure 1). Youth aged 12-17 have the highest rates of ADHD, coming in at 13.5% in 2016.33 In adults, the lifetime prevalence of ADHD is 8.1%.44
FIGURE 1: INCREASE IN U.S. RATES OF CHILDREN WITH ADHD FROM 1997-2014.
From General Prevalence of ADHD. (2020). Redrawn from https://chadd.org/about-adhd/general-prevalence/
Additionally, 25% of children have some form of anxiety,55 and anxiety affects 20% of American adults,66 with just over one-third getting treatment.77
While behavioral health rates are on the rise, currently, in-network insurance coverage for behavioral health treatment is falling compared to coverage for primary care.88 This means that options for ADHD and other behavioral health treatment are fewer, less accessible, and less affordable.
In light of a recent groundbreaking report, insurance companies have more reason than ever to fast-track approval of effective evidence-based behavioral health interventions. Beyond access to coverage, not doing so could also be costing payers billions of dollars.
In August 2020, Milliman Inc. provided an analysis of healthcare spending on 21 million commercially-insured individuals. Strikingly, the most expensive 10% of patients accounted for 70% of annual total health care costs; and within this high-cost group, 1.2 million individuals received a behavioral health diagnosis and/or treatment. Though this subgroup represented just 5.7% of the study participants, they accounted for 44% of annual total health care costs for the entire study population. Tragically, 50% of these individuals received less than $95 in behavioral health treatment annually, including prescription drugs.99
Former CEO of Magellan Health and advisor to The Path Forward mental health care reform initiative, Henry Harbin, MD, stated, “Tremendous savings and improved outcomes are achievable if these individuals are identified early and provided with prompt evidence-based behavioral health treatment”.1010
The Case for NFB
NFB has a 70-year history and thousands of studies, many of which focus on treating behavioral health conditions and validate its effectiveness at improving behavioral health and brain fitness. The weight of the research shows NFB to be efficacious and effective at treating ADHD.
Including in-network reimbursement of NFB treatment for ADHD would be adding a non-invasive, relatively inexpensive, efficacious and effective intervention to the set of available treatments for children and adults with behavioral health disorders.
Over the past 11 years, at least four major research reviews by leading researchers in the U.S. and internationally have shown NFB to be an efficacious intervention for the treatment of ADHD. Several studies have found NFB improvements lasting up to a year post-treatment, which compares positively to improvements from ADHD medication which tend to end immediately with the conclusion of treatment.
Neurofeedback (NFB) has also been found to be effective as a treatment for anxiety. NFB equipment is FDA-approved for relaxation training. Research shows that relaxation is a primary treatment for anxiety and other symptoms of stress- and adjustment-related disorders. As a non-pharmacological option, NFB can be used to treat symptoms of anxiety.
For an overview of neurofeedback’s recent evidence for treating ADHD and anxiety, click here.
Compliance and the Mental Health Parity and Addiction Equity Act (MHPAEA)
Beyond the impetus to provide equal access to and coverage of behavioral health interventions such as NFB, insurance providers may want to consider enforcement of the Mental Health Parity and Addiction Equity Act (MHPAEA), which requires group health plans with mental health and substance use disorder benefits to offer equal coverage for these disorders as they do for medical/surgical benefits.1111
Recently, the Illinois Department of Insurance (IDOI) fined five major insurance companies for violating the 2008 MHPAEA. CIGNA Healthcare of IL, United Healthcare, CIGNA Health and Life, Health Care Service Corporation (Blue Cross Blue Shield of Illinois), and Celtic were fined more than $2 million for violations of the MHPAEA. Payers are well-served staying in compliance with MHPAEA.
For more in depth information, read a summary of recent evidence that supports NFB to treat ADHD and anxiety, or download BrainFutures’ full NFB report.
[1] Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD) National Resource Center on ADHD. (n.d.).General Prevalence of ADHD. Retrieved from https://chadd.org/about-adhd/general-prevalence/
[2] CDC. (2018, September 21). Data and Statistics About ADHD. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/adhd/data.html
[3] Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD). (2020). General Prevalence of ADHD. https://chadd.org/about-adhd/general-prevalence/
[4] NIMH » Attention-Deficit/Hyperactivity Disorder (ADHD). (2017, November). Nih.Gov. Retrieved from https://www.nimh.nih.gov/health/statistics/attention-deficit-hyperactivity-disorder-adhd.shtml
[5] CDC. (2018, December 20). Data and Statistics on Children’s Mental Health. Centers for Disease Control and Prevention. https://www.cdc.gov/childrensmentalhealth/data.html
[6] NIMH » Major Depression. (2019, February). Nih.Gov. Retrieved from https://www.nimh.nih.gov/health/statistics/major-depression.shtml
[7] Anxiety and Depression Association of America | Facts & Statistics. (n.d.) Adaa.Org. Retrieved from https://adaa.org/about-adaa/press-room/facts-statistics
[8] Melek, S., Fsa, Maaa, S., Davenport, M., & Gray. (2019). Addiction and mental health vs. physical health: Widening disparities in network use and provider reimbursement A deeper analytical dive and updated results through 2017 for 37 million employees and dependents. Retrieved from http://assets.milliman.com/ektron/Addiction_and_mental_health_vs_physical_health_Widening_disparities_in_network_use_and_provider_reimbursement.pdf
[9] Davenport, S., Gray, T.J., and Melek, S.P. (2020, August 13). How do individuals with behavioral health conditions contribute to physical and total healthcare spending? Milliman, Inc. Retrieved from https://www.milliman.com/en/insight/How-do-individuals-with-behavioral-health-conditions-contribute-to-physical
[10] The Mental Health Association of Maryland, MidAtlantic Business Group on Health. (2020, August 13). Groundbreaking New Study Reveals People Diagnosed with Both Behavioral and Physical Health Conditions are Among the Highest-Cost Patients, Yet Less than 5% of Health Care Spending is Directed Toward Behavioral Health Treatment [Press release]. Retrieved from https://www.mhamd.org/news/2020-milliman-press-release/
[11] CMS.gov. (n.d.). The Center for Consumer Information & Insurance Oversight, Mental Health Parity and Addiction Equity Act (MHPAEA). Retrieved from https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/MHPAEA